Supersizing Pregnancy Care: the Dawn of Bariatric Obstetrics?
Monday, April 7, 2008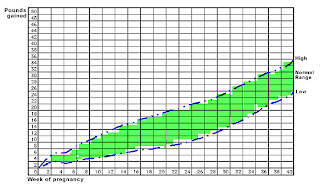
Last week’s issue of the New England Journal of Medicine features an article by Susan Chu and colleagues from the US Centers for Disease Control and Prevention (Atlanta, GA) on the impact of obesity on health care during pregnancy.
Dr. Chu and colleagues examined 13,442 pregnancies (2000-2004) according to pre-pregnancy BMI. After appropriate corrections for confounders, hospital stay for delivery was significantly greater by approximately a full day among women with obesity than in normal weight women. Most of the increase in length of stay associated with higher BMI was related to increased rates of cesarean delivery and obesity-related high-risk conditions.
A higher-than-normal BMI was also associated with significantly more prenatal fetal tests, obstetrical ultrasonographic examinations, dispensed medications, telephone calls to obstetrics, and prenatal visits with physicians. Thus clearly, obesity during pregnancy is associated with increased use of health care services.
Obesity in pregnancy is not a topic that is discussed much in the media. I first became aware of the magnitude of this problem, when I was approached by the obstetrics folks from the McMaster University Hospital (Hamilton, Ontario) who found themselves looking after an increasing number of severely obese expecting mothers. This contact led to the initiation of a working group on bariatric nursing that devised protocols for looking after large and very large mothers.
I further realised the importance of this issue when I heard about the apparently close link between maternal obesity and the risk for both the mother and infant and the fact that obesity during pregnancy may set up the infant for future obesity through epigenetic programming. As I have blogged before, limiting weight gain during pregnancy in overweight and obese mothers may be a first step towards preventing childhood obesity.
Given that there are around 13,000 babies born in the Capital Health Region every year, about 10% of these to mothers with pre-pregnancy BMI>30, the finding of Dr. Chu et al., if translated to our region, could mean as many as 1,500 or so extra days in hospital for new mothers, much of this due to obesity-related risk. Obviously more screening tests, more frequent prenatal visits and more medications would add to the costs.
Clearly, the issue of increasing weights and weight gain in women of child-bearing age is a public health issue whose consequences and impact have yet to be fully appreciated.
As these issues affect both mothers and infants, it would not be a bad place to focus prevention measures for best impact.
AMS
Edmonton, Alberta


