Mitochondria and Obesity Revisited
Tuesday, July 15, 2008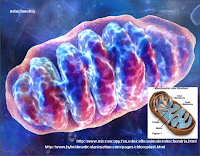 Several months ago I blogged about the results from a Finnish twin study that found lower mitochondria numbers and disturbed mitochondrial energy metabolism activity in fat cells from identical twins who were leaner than their genetically identical co-twins. These impairments correlated with critical clinical measures of obesity including liver fat accumulation, reduced whole-body insulin sensitivity, hyperinsulinemia, hypoadiponectinemia and adipocyte hypertrophy.
Several months ago I blogged about the results from a Finnish twin study that found lower mitochondria numbers and disturbed mitochondrial energy metabolism activity in fat cells from identical twins who were leaner than their genetically identical co-twins. These impairments correlated with critical clinical measures of obesity including liver fat accumulation, reduced whole-body insulin sensitivity, hyperinsulinemia, hypoadiponectinemia and adipocyte hypertrophy.
In this month’s issue of OBESITY, Tomas Gianotti and colleagues from the University of Buenos Aires, Argentina, report a significantly lower mitochondrial-to-nuclear DNA ratio (mtDNA/nDNA) in insulin resistant (IR) adolescents recruited out of a subset (n=175) of a cross-sectional, population-based study of 934 high school students. In this study, the mtDNA/nDNA ratio was also inversely correlated with HOMA index, a crude but simple measure of insulin resistance.
This study is very much in line with the notion that obesity-prone individuals may have impaired mitochondrial number and/or function resulting in increased risk for obesity.
From the aforementioned twin study, we know that the decreased number and function is not corrected by weight loss.
Indeed the question is whether or not mitochondrial number and function can be increased by prescribing higher activity levels? If yes, how much activity will be needed to reverse these changes? And most importantly, will people with impaired mitochondrial function actually be able to enjoy exercise enough to actually stick with this prescription?
Perhaps it is not obesity that causes impaired mitochondrial function but rather impaired mitochondrial number and/or function that predisposes to obesity. This impairment could be genetic but also due to intrauterine programing or perhaps simply luck of the draw (remember – all mtDNA comes from your mom).
Of course this is not an “excuse” for obesity as is often misinterpreted when data on the genetics and biology are presented. However, it is clear that if you have impaired mitochondrial number and/or function you are much more likely to become obese in an environment that promotes sedentariness than if you were dependent on physical activity to meet your basic needs for survival.
Remember, there were times, not too long ago, when people were actually paid to be physically active. Today, choosing to be physically active actually costs money (not to mention time).
AMS
Edmonton, Alberta


